Itch Explained
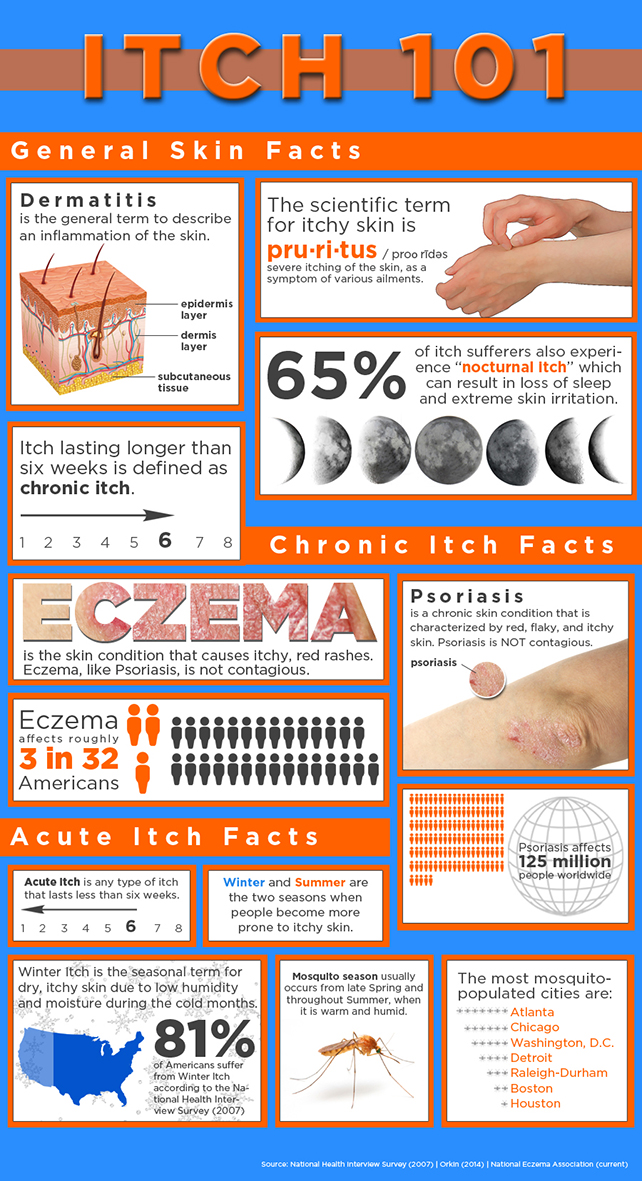
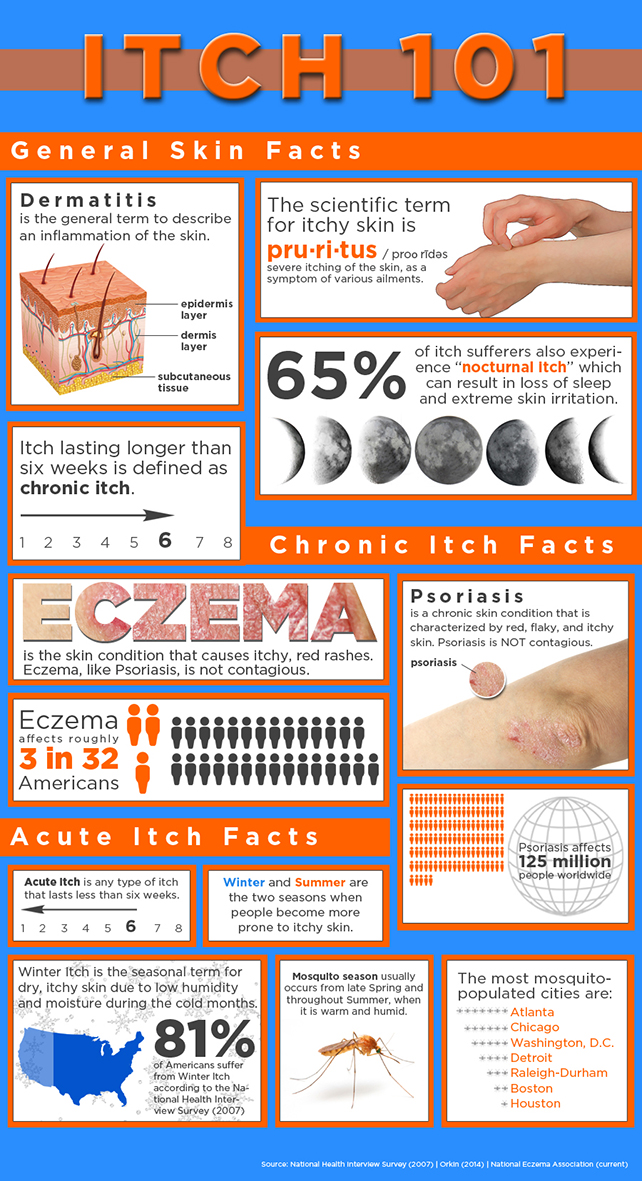
We created this handy infographic to help you understand the basics of itch.
ifz_adm1 Itch 101, Itch Basics
We created this handy infographic to help you understand the basics of itch.
ifz_adm1 Itch 101, Itch Basics itch101, itch101 featured

We’ve all had those nights where time keeps tick-tocking closer to the morning light but sleep is nowhere to be found. Now, imagine in your restlessness that you are super itchy on top of this.
Believe it or not, nocturnal itch is a “thing.” Majority of patients with inflammatory skin conditions (such as eczema, and psoriasis) experience increased itching at night. Nighttime itching can cause you to scratch in your sleep, which in turn irritates your skin and leads to sleep loss.
So – why do we itch more at night? Well, the short answer is, the doctors are unsure.
“Previously, the main explanation for nocturnal itch was that people are busier during the day, surrounded by distractions that take their minds off the itch but that is no longer the case,” said Gil Dr. Yosipovitch, Director of the Itch Center at Temple University Medical School and member of the Cosmederm Bioscience Scientific Advisory Board. “We are gaining a better understand of nocturnal itch and believe that variety of factors can lead to it.”
One theory explains that your skin temperature can fluctuate with your circadian rhythms – the changes in your body over a 24-hour period that often dictate sleep patterns. Your skin actually loses more water during the night, which can lead to increased itch. Also chemicals that induce itch may be increased at night time.
While the “usual suspects” of itch treatments can help nocturnal itch, doctors will also sometimes prescribe medications that can have a sedative effect.
“Drugs such as sedating anti-histamines such as Hydroxyzine as well as ant-epileptic drugs such as Gabapentin and Pregabalin and types of anti-depressants such as mirtazapine that cause sedation may help the patients have better sleep and less scratching at night time,” said Yosipovitch.
References: http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-0280&html=1

ifz_adm1 Itch 101, Itch Basics, Managing Acute and Chronic Itch, Sidebar Feature featured, itch101, manage featured

Living with sensitive skin can be difficult in today’s world. With the plethora of skin care products available to you, navigating through the ingredient list to discern what causes your irritation can be aggravating. Depending upon the level of your skin’s sensitivity, your reaction to an allergen can be a minor skin rash or a traumatizing allergic reaction requiring immediate medical attention.
There are four categories of sensitive skin:
Many people determine they have sensitive skin if they frequently experience allergic reactions that can produce redness, rashes or acne outbreaks after using certain soaps or lotions. Some people have severe sensitive skin where they experience redness and tenderness with the slightest touch, inhibiting their ability to live life to the fullest.
The number of people who say they have sensitive skin has increased over the last 30 years. Some doctors credit this to factors such as climate and seasonal conditions, which can have a direct influence on one’s skin. Environmental factors such as UV exposure, frequent contact with water, soaps and cleansers can break down the skin’s natural barrier and leave skin dry, itchy and red.
Some common causes for sensitive skin include:
Allergies: Allergies can be caused by foods you digest or chemicals found in common skin care products. Allergic reactions can include itching, rashes, hives, runny nose, itchy or watery eyes, exhaustion, nausea, swelling, redness, pain, stomach cramps diarrhea and vomiting.
Genetics: Research studies have concluded that fair-skinned people tend to develop more severe cases of skin sensitivity. This may be due to the lack of melatonin within their skin, which acts as protection from harmful environmental factors.
Poor Digestion: Poor digestion can also play a role sensitive skin. People with poor nutrition tend to have an inflamed digestive tract. This kind of inflammation can affect many other organs including skin. Studies have also shown that poor nutrition can lead to sluggish elimination. If toxins in you body are not flushed out properly through the digestive tract, they are more likely to penetrate the skin.
Treatments for sensitive skin:
If you have sensitive skin you will want to first determine the source of your reactions. If you are suddenly having acne breakouts, they may be caused by a new cleanser, lotion or even a new food you are eating. The best way to determine what might be causing your allergic reaction is to watch out for certain patterns.
Once you have discovered what might be causing your skin to react, avoid using that product or any other product with those ingredients. If your skin is dry and irritated, finding a thick moisturizing cream will help protect your skin’s barrier allowing it to heal. Using TriCalm hydrogel will help stop the itch, providing you and your skin relief.
ifz_adm1 Itch 101, Itch Basics, Manage My Itch, Managing Acute and Chronic Itch

In the previous post on itchy skin, we discussed the data on the prevalence of itch and the lack of satisfactory itch treatments. Here, we take a deeper dive into available itch treatments and their efficacy and safety.
Topical Antihistamines
There are more than 70 distinct chemicals that are believed to mediate itch symptoms. Histamine is the most well-known of these itch and inflammation-triggering chemicals. Histamine binds to the type C nerve receptors and triggers the brain to produce an itch sensation, so antihistimines block the histamine from binding to the receptors.
A risk associated with using topical antihistamines is triggering a secondary allergic reaction identical to that experienced with poison ivy. Another common side effect of antihistimines is drowsiness.
Notwithstanding, the lack of effectiveness of topical antihistamines and their safety concerns, topical antihistamines like Benadryl™ continue to be widely sold and, presumably due to their placebo effect, consumers continue to purchase them.
Topical Local Anesthetics
Topical anesthetics are a common treatment for itch, and they essentially act as numbing agents to quiet itch symptoms in an affected area. Active ingredients like benzocaine and lidocaine are commonly used in over-the-counter products. However, benzocaine is one of the most likely ingredients to cause a secondary allergic reaction identical to that experienced with poison ivy/oak/sumac. It’s estimated that 1% of benzocaine users may experience this.
Another concern with topical anesthetics is the potential for systemic absorption. Although an unlikely occurrence when used as directed, applying topical anesthetics to large areas of the body repeatedly poses a danger of systemic toxicity, essentially drug overdose.
Risks:
Glucocorticoids (i.e., Cortizone-10)
Working on reducing the inflammation that can cause itch, these products have no direct effect on the sensory irritation, i.e., the itching, burning and stinging sensations. So they don’t work right away, they take a day or more to produce any significant benefit, and since they don’t target the itch nerves directly, they are ineffective on many common itch conditions, such as acute contact dermatitis – like poison ivy, jewelry allergies, bug bites and atopic dermatitis.
Risks:
Topical Counterirritants
These products, with ingredients such as menthol and camphor, provide no direct itch relief. Rather, they activate other nerve subsets that send a cold or “cooling” sensation to the brain, thus distracting you from the itch. They have limited effect and last only for a limited time.
[1] American Pharmaceutical Association’s Handbook of Nonprescription Drugs
Why do we still suffer from itchy skin?
Itch. It’s something I’d venture to say we’ve all experienced. When surveyed, 78% of adults reported experiencing some type of itch or skin irritation within the past year.[1] Itch, in particular, can range from as mild and temporary as a mosquito bite to as severe and chronic as psoriasis. In fact …
“… although itching is popularly perceived as a minor social or even humorous disability, it is frequently so severe and intractable as to cause the sufferer abject misery or even suicidal inclination.”
– Fitzpatrick’s Dermatology in General Medicine
Can you imagine having itch so severe you can’t sleep, think, or even function? Unfortunately for some this is a daily reality. But for most of us, itch is just an occasional annoyance. And about 49% of us head to the drugstore for a solution.[2]
Considering there are multiple triggers for itch, it is surprising how lacking the offerings are in terms of effective itch treatments. Consider this: The need for new and improved itch treatments was famously demonstrated in a 1964 study where 12 patients were treated with four different oral anti-itch medications in rotation so that each of them received each treatment during the study. The most effective treatments were 66% effective in relieving itch symptoms! And only 16% of treatments produced side effects like nervousness or grogginess, not bad. BUT here’s the catch … all the treatments were placebos!
So that means a placebo performs as well as, if not better than, many medications at relieving itch. Fitzpatrick’s Dermatology in General Medicine authors state,
“as of 1998, no specific anti-itch drug of proven efficacy was available.”
Even in 2003, leading itch scientists stated, “Currently there are no satisfactory selective anti-itch treatments.”[3]
And when it comes to over-the-counter remedies, in a 2012 Harris survey, more than one in three people surveyed said they were not satisfied with OTC options available to treat itch.[4]
Here’s a quick breakdown of what happens when your skin itches. Your skin has two types of itch nerve receptors, A-Delta nerves that produce the sharp, pricking pain of a needle, and type C nerves that cause itching, burning, stinging sensations and inflammation. Irritants such as chemicals, allergens or insect bites easily activate type C nerves. When the itch stimulus enters the skin, type C nerves send an itch signal to the brain and trigger the body to release histamine that dilates the blood vessels, causing redness and swelling.
In the next post, we’ll cover common topical anti-itch treatments and their relative efficacy and safety.
[1] 2012 Mintel Medicated Skincare Report
[2] Ibid.
[3] Itch Associated with Skin Disease: Advances in Pathophysiology and Emerging Therapies.
[4] 2012 Harris Interactive online survey of 2,213 U.S. adults aged 18+

ifz_adm1 Bug Bites, Itch 101, Itch Basics bug bites

Planning your next camping trip this summer? Check out our list of environmental hazards you should avoid this summer
Poison Ivy grows as vines or low shrubs in most climates. Each leaf on a poison ivy plant has three smaller leaflets. Contact with any part of the poison ivy plant can cause red, swollen skin, blisters and severe itching, sometimes within hours after exposure. Learn more about poison ivy.
Ragweed plants usually grow in rural areas or open meadows. Ragweed pollen is a primary cause of hay fever (allergic rhinitis). For those who are sensitive to ragweed, ragweed exposure can also cause a rash. You might notice small, itchy bumps and blisters after you come in contact with the plant. A ragweed rash usually develops within two days of exposure and resolves on its own within two to three weeks, as long as you avoid any additional ragweed exposure.
Wild parsnip grows in sunny areas, often along highways and in prairies. The plant bears large, flat clusters of yellow-green flowers on a thick stem. Sap from the wild parsnip plant—along with exposure to sunlight—can cause a burn-like reaction on the skin. Within a day after exposure, the skin turns red and may blister. The affected area, which feels like a mild to severe sunburn, often turns brown. This discoloration sometimes lasts for months.
Swimmer’s Itch is an itchy rash caused by certain parasites that normally live on waterfowl and freshwater snails. On warm, sunny days—especially in calm freshwater lakes or ponds-these parasites are released into the water and burrow into your skin. Once the parasites die you’re left with itchy, red, raised spots on your skin.
Chiggers are tiny mites found in tall grass and weeds. If you brush against infested plants, chiggers may bite and attach to your skin. After a few days the chiggers will fall off, leaving behind red, itchy skin.
Sun rashes Many people are highly susceptible to sun rash. A sun rash occurs from over exposure to intensive sunlight or from certain medications such as anti-inflammatories or antibiotics. An allergic reaction to the sun can cause solar hives, which are raised, itchy, red welts that appear five to 10 minutes after initial sun exposure.
To prevent sun rash, avoid substances that may lead to a sun rash and always wear broad-spectrum sunscreen containing UVA and UVB rays with a sun protection factor (SPF) of 30 or higher.
Also, wearing tightly woven clothing that covers your arms and legs and a broad-brimmed hat will also help eliminate sun exposure.
Fire burns What is the first thing we think of when camping? Campfire and marshmallows! One thing we forget is how easy it is to burn yourself while camping. You should never light a campfire by throwing a lighted match on timber doused with lighter fluid. Always keep an eye on young children during a campfire. If you do happen to get burned the affected skin should be cooled by placing it under cold running water for at least one hour.
ifz_adm1 Itch 101, Itch Basics

Itch. It’s something I’d venture to say we’ve all experienced. When surveyed, 78% of adults reported experiencing some type of itch or skin irritation within the past year.[1] Itch, in particular, can range from as mild and temporary as a mosquito bite to as severe and chronic as psoriasis. In fact …
“… although itching is popularly perceived as a minor social or even humorous disability, it is frequently so severe and intractable as to cause the sufferer abject misery or even suicidal inclination.”
– Fitzpatrick’s Dermatology in General Medicine
Can you imagine having itch so severe you can’t sleep, think, or even function? Unfortunately for some this is a daily reality. But for most of us, itch is just an occasional annoyance. And about 49% of us head to the drugstore for a solution.[2]
Considering there are multiple triggers for itch, it is surprising how lacking the offerings are in terms of effective itch treatments. Consider this: The need for new and improved itch treatments was famously demonstrated in a 1964 study where 12 patients were treated with four different oral anti-itch medications in rotation so that each of them received each treatment during the study. The most effective treatments were 66% effective in relieving itch symptoms! And only 16% of treatments produced side effects like nervousness or grogginess, not bad. BUT here’s the catch … all the treatments were placebos!
So that means a placebo performs as well as, if not better than, many medications at relieving itch. Fitzpatrick’s Dermatology in General Medicine authors state,
“as of 1998, no specific anti-itch drug of proven efficacy was available.”
Even in 2003, leading itch scientists stated, “Currently there are no satisfactory selective anti-itch treatments.”[3]
And when it comes to over-the-counter remedies, in a 2012 Harris survey, more than one in three people surveyed said they were not satisfied with OTC options available to treat itch.[4]
Here’s a quick breakdown of what happens when your skin itches. Your skin has two types of itch nerve receptors, A-Delta nerves that produce the sharp, pricking pain of a needle, and type C nerves that cause itching, burning, stinging sensations and inflammation. Irritants such as chemicals, allergens or insect bites easily activate type C nerves. When the itch stimulus enters the skin, type C nerves send an itch signal to the brain and trigger the body to release histamine that dilates the blood vessels, causing redness and swelling.
Topical Antihistamines
There are more than 70 distinct chemicals that are believed to mediate itch symptoms. Histamine is the most well-known of these itch and inflammation-triggering chemicals. Histamine binds to the type C nerve receptors and triggers the brain to produce an itch sensation, so antihistimines block the histamine from binding to the receptors.
A risk associated with using topical antihistamines is triggering a secondary allergic reaction identical to that experienced with poison ivy. Another common side effect of antihistimines is drowsiness.
Notwithstanding, the lack of effectiveness of topical antihistamines and their safety concerns, topical antihistamines like Benadryl™ continue to be widely sold and, presumably due to their placebo effect, consumers continue to purchase them.
Topical Local Anesthetics
Topical anesthetics are a common treatment for itch, and they essentially act as numbing agents to quiet itch symptoms in an affected area. Active ingredients like benzocaine and lidocaine are commonly used in over-the-counter products. However, benzocaine is one of the most likely ingredients to cause a secondary allergic reaction identical to that experienced with poison ivy/oak/sumac. It’s estimated that 1% of benzocaine users may experience this.
Another concern with topical anesthetics is the potential for systemic absorption. Although an unlikely occurrence when used as directed, applying topical anesthetics to large areas of the body repeatedly poses a danger of systemic toxicity, essentially drug overdose.
Risks:
Glucocorticoids (i.e., Cortizone-10)
Working on reducing the inflammation that can cause itch, these products have no direct effect on the sensory irritation, i.e., the itching, burning and stinging sensations. So they don’t work right away, they take a day or more to produce any significant benefit, and since they don’t target the itch nerves directly, they are ineffective on many common itch conditions, such as acute contact dermatitis – like poison ivy, jewelry allergies, bug bites and atopic dermatitis.
Risks:
Topical Counterirritants
These products, with ingredients such as menthol and camphor, provide no direct itch relief. Rather, they activate other nerve subsets that send a cold or “cooling” sensation to the brain, thus distracting you from the itch. They have limited effect and last only for a limited time.
[1] American Pharmaceutical Association’s Handbook of Nonprescription Drugs
[1] 2012 Mintel Medicated Skincare Report
[2] Ibid.
[3] Itch Associated with Skin Disease: Advances in Pathophysiology and Emerging Therapies.
[4] 2012 Harris Interactive online survey of 2,213 U.S. adults aged 18+

ifz_adm1 Itch 101, Itch Basics itch101 featured

Pruritus. While it might sound like a strange disease, you might be surprised to find it’s actually quite common.
Simply put, pruritus is the medical term for “itchy skin,” which can be a symptom of many different things – from other medical conditions like psoriasis and eczema, to environmental conditions like allergies, bug bites, and drug reactions. Irritation from contact with fabrics, cosmetics, or other substances also can lead to itching.
Itchy skin is one of the most frequent symptoms in dermatology. Chances are, if you’ve ever felt scaly from dry skin, you’ve experienced pruritus. You might also know that being itchy can be extremely uncomfortable and have an impact on your everyday life. Poor sleep and problems concentrating are just two things that people suffering from a bad itch have experienced. For some people, having a chronic form of itch has even led to symptoms of depression.
So – what can be done to help pruritus? While it can be tempting and might make you feel temporarily relieved, scratching can actually damage the skin and increase your skin’s inflammation, so doctors do not recommend it as a solution. However, there are several treatment options available (both over-the-counter and by prescription) that can help ease the discomfort associated with itch. Generally speaking, if the itch lasts more than two weeks and self-treatment has not worked, it may be time to speak with your doctor or dermatologist.
References: Mayo Clinic, Annals of Dermatology/Chronic Pruritus: Clinics and Treatments, Cleveland Clinic, International Forum for the Study of Itch; JAMA Dermatology/ The Impact of Pruritus on Quality of Life